It is the longest time since a post. Because of reasons of course. All of the boring reasons.
And I would like to pretend that this post heralds the resumption of really regular posts. It does not.
This site is a great location after doing a talk though because I can easily put up all of the links and bits and pieces that went into it. Much more useful and open than a set of slides which have 3 words each on them.
This post has turned up because of a talk I was asked to do for 2nd part exam prep for clever anaesthetists in South Africa. And I was asked to talk about acquired tracheo-oesophageal fistula and button batteries. And while I like a trip down memory lane this sort of means that the last two posts both look pretty much the same thing. There were things to update so and that makes this genuinely new. I guess if the next post is also about button batteries, I may have to turn it into a button battery site.
Things Happening Everywhere
This was a talk for the middle of the day and the end of the night. In fact it was a talk for lots of different places all at once about things that can cause all types of problems almost all at once – button batteries. Perhaps part of the reason I was asked to do this talk at all was that … well I am bad at saying no in all of the different versions of time and space.
And I can totally understand why people are very occupied with the horror inflicted by button batteries, including the acquired tracheo-oesophageal fistulas they create. We’re seeing far more serious injuries in recent years. Back in 1992 the major morbidity rate was 0.08% and there were no fatalities. Fast forward a couple of decades and that major morbidity rate is 0.66% and that just means that inevitably we’re seeing serious things.
And the thing about medicine is something that happens 0.66% of the time feels major when you, or someone you know has been there for the event. Seeing serious complications has a way of sticking with you.
Plus there’s at least one significant reason for the spike in morbidity – bigger batteries. In 2006 the 3 V Lithium battery, usually measuring above 20 mm in diameter, hit the market. It’s said that this relatively chunky and more powerful battery hitting the market made a difference – in fact in some series the rate of major morbidity or mortality in those under 6 ingesting one of these batteries is as high as 12.6%.
So let’s turn to a story. Or better yet 3 stories in 3 realities. Because every time we make a choice that creates a fork we create another universe to tangle with. A wholly encapsulated version of ourselves making slightly different choices and facing slightly different challenges and eating burgers with meat that’s meat but also meat that is weird in each of those locations. (Yes, the talk was late at night and a little bit of multiverse theory that probably doesn’t accord entirely with actual multiverse theory is a way to keep yourself awake.)
So here we arrive in universe 1.

The First Version
You know this one. It’s about 18:00. You’re at Nelson Mandela Children’s Hospital. The colours are big. The kidney dishes fly as butterflies in the foyer. A 2 year old turns up. This isn’t random. A parent brought them because they’re a little worried about the possibility that they’ve swallowed something. A button battery.
It’s not a huge history. The child was playing in the lounge room with a bunch of their siblings toys. A lot of work was being done one very other room. Bu then it became apparent that there was a battery missing from one of those toys.
So the first question to ask here is ‘Does this even seem like it could be real?’ After all, where’s the witnessed ingestion? Where are the symptoms? Shouldn’t this be obvious?
Well it turns out that a story that’s not much of a story is actually pretty common.
There’s an Australian paper put out by the New South Wales statewide poisons service looking at 578 total battery exposures between November 2015 and May 2017. The median age was 23 months. They looked at 578 exposures and in 188 of those cases they were able to follow up to get a story about the presenting history. That’ll show the story of huge symptoms or some history of ingestion, right?
Well no. Because those are not things. As it turns out only 4% were associated with the ingestion being witnessed. That’s not a huge number. In 40% the only history was that a battery was noted to be missing.
A similar story emerges looking at a paper out of Saudi Arabia published in 2019 but looking at cases of foreign bodies from 2007-2016. This one looked at the story for 436 kids. 22.6% of the cases were coins and 19.5% were batteries. 76.1% of that total number of patients were asymptomatic at presentation.
Understanding these features is really important. One of the things that also emerged in the Australian paper was that triage responses were really inconsistent. Frequently a real lack of urgency in trying to figure out what was going on, an assumption that without a clear history the risk was probably just not there, was identified in the cases they were looking at. That risk assessment is based on an assumption not in the evidence – there will be enough clues to make it clear when you should actually worry.
In reality what is needed is a high index of suspicion because a clear history is hard to arrive at. You should definitely be extra worried if there’s:
- A story of refusing oral intake.
- Dysphagia.
- Upper gastrointestinal haemorrhage.
- Any evidence of chest pain, drooling or airway obstruction.
But some history should still be enough to take things seriously.
It’s an Interactive Universe
At this point we went to the polls. In fact we’d tested out if online polling would be feasible at the start by checking via Slido how people were feeling (turnout 28% of people felt comfortable confessing they were full of lunch and just wanted to curl up and go to sleep). Also it appears that 62% of registrars in the audience feel that examiners are reasonable people, and not demons from the Neverworld come to unleash pain. Let’s hope they’re right, not the 8% who think examiners are actual demons .
It was a simple question to contemplate “What now?” and the overwhelming response from 84% of people was ‘X-ray thanks’ rather than enjoy multiverse 1 dinner, or a CT scan or wait and see. This seems like a pretty understandable response. Probably quicker to arrange than a CT and still likely to reveal useful stuff while imposing less of a radiation load.
And it’s definitely worth doing something because there are established risk factors here – the patient is under 6, it could have been more than a couple of hours (because 2 hours is more than enough time for damage to occur) and if it is a battery, what if it’s bigger than 20 mm?
So you want an investigation like this (particularly if you’re a speaker looking to push things along…)

There are a few key things on the X-ray of course (I’m just going to go right ahead and assume you can spot the thing that is not supposed to be there):
- Location – there are classic points of particular concern because they represent points where a button battery might get stuck and can guide you as to which bits of the anatomy are at risk. The region of the clavicles corresponds with the cricopharyngeus, and a pretty high point in the airway. Head down a little lower to the vicinity of the carina and you’re in territory that’s also perilously close to the arch of the aorta. A bit lower and you’re getting to the pause point at the lower oesophageal sphincter.
- Identity – while you can’t always spot the nature of a foreign body, there is a chance you may be able to pick out the halo sign that is characteristic of a button battery. It’s the shadow created by the structure of the thing itself (unlike the homogenous disc of a coin as a comparator).

- Direction – this is a 3rd key item for a button battery. The damage created by a button battery occurs at the negative pole. The negative pole is the surface with less width on it. So the direction it is facing (best picked on a lateral) gives a pretty good clue as to where tissues are getting injured. For example if it’s around the carina or left main bronchus and the negative pole is facing to the patient’s spine, that big vessel is at risk. If it’s facing the sternum, the airways are in the firing line.
So now that we know it’s a ‘thing’, what are the priorities?
The first one is to move quickly. The aim is removal of that button battery in under 2 hours. And that’s just about minimising damage. In a paper on anaesthetic management of button battery ingestion Ing et al even note the option of introducing the equivalent of a trauma team response for button battery scenarios because you need to move the patient that quickly. That same suggestion of timeline is in relevant North American guidelines and the soon to be published European guidelines.
2 hours. Get it done.
The other priority is to minimise any damage. And for that there is only one obvious option.

While there were early theories that the extraordinary damage caused by batteries might be related to direct pressure or leak of battery acids, it is now understood that the issue occurs at the negative pole where generation of a local current generates hydroxide ions and lead to an alkali burn. Within a short period of time the pH locally can get up around the 13 range. It only takes about 15 minutes to start seeing some evidence of tissue damage when it comes in contact with a button battery.
Honey appears to coat the battery and prevent generation of those hydroxide ions. In vitro studies looking at cadaveric porcine oesophagus demonstrated that both honey and sucralfate do a better job of preventing tissue damage than saline. Similar findings have been confirmed when applied to living pigs and subsequently checked. It appears there is probably benefit for longer than you might expect, but given the concern that with increasing time comes increasing risk of perforation, the suggestion is that this is a manoeuvre best reserved for the first 12 hours.
Of course you can use that sucrafalate. But as it seems like most kids (over 1 once it’s safe) would probably take honey onboard, honey seems logical.
Then the thing that happens next is someone has to get it. Because you can guarantee someone will pretty much need to get it. In a retrospective review of cases from South Africa looking at cases between 2010 and 2015, they reported 462 non-food objects causing problems. In this series only 4.8% of those were batteries. However 36.4% of those patients presenting with a battery ingestion needed a general anaesthetic to try and sort it out (compared to around 15% in the total series).
Now, that X-ray itself might well have helped with the ‘who?’ bit. The most likely thing if you’re dealing with something around the clavicles or above is that ENT are the team to grab that pesky thing. That’s what 83% of the audience thought too. (I’ll note it is reasonable to think you may want to look at the time of intubation just in case you find something to grab. A videolaryngoscope can be a really useful option in that context so everyone can see what you’re seeing.)
For foreign bodies lower than that it becomes even more of a discussion as to whether it’s an ENT grab the thing scenario or a gastroenterology grab the thing scenario. Either way with a relatively tight timeframe it’ll be that group getting it done and active chat is needed.
There is a chance that the choice made when it comes to retrieving that foreign body will also have an impact on some choices when it comes to induction and choice of airway. Chances are that whatever pathway you go down, you’ll be looking at placing an endotracheal tube, in a rapid sequence fashion. But it is probably worth asking any involved ENT types if they want to look at the airway, just in case there’s a need to treat it more like rigid airway endoscopy.
The final point in this sequence is that looking after the tissues doesn’t stop at removing the battery. The pH in those tissues still needs treating. All it takes is 50-150 mL of 0.25% acetic acid irrigation.
And while that’s happening, a 2 year old comes to Chris Hani Baragwanath Hospital in multiverse number 2.

And Now For Something a Little Different
You will understand that this multiverse is the one you created that one time at Uni when instead of getting up in the morning to get those bins out when you heard the garbage truck (you were definitely up studying) you decided to sleep in.
And in this particular multiverse at the exact same moment as a patient turned up to multiverse 1 Nelson Mandela Children’s Hospital this 2 year old arrives but seems to have had a vomit. And maybe that vomit had some blood in it. On reflection this one has been playing with their siblings toys a lot over the last few days.
Now maybe it was because they just had a sense that a high index of suspicion when kids come in with stories like this or maybe it was directly prompted by some weird multiverse entanglement but someone has gone to the effort to grab an X-ray.

Now obviously that’s convenient for a whole thing on button batteries, but it’s also highly relevant to consider the timeline here. Our goal is to minimise tissue damage so we need it out within 2 hours, so what are we waiting for?
Well, the thing here is there is even more uncertainty about the history but also at least some symptoms suggestive of something else going on. Bleeding suggests something is already damaged and you’d have to wonder about the chance of perforation or something similar.
Soto et al published work looking at 290 severe or fatal ingestions, and in 189 of those cases there was some form of oesophageal perforation. In 149 they were able to pin down the time of ingestion to time of peroration. 2% had less than 24 hours exposure. On day 2 and 3 the rates the cumulative rate hit 7.4% and 10.1%. It was at 3 days exposure and up that perforations really became more evident. By day 3 post-exposure, 26.8% of perforations had declared themselves. (It is worth noting that there is also a risk of perforation after removal so patients can turn up weeks after an ingestion and removal with a perforation – this makes those initial efforts to minimise tissue damage even more obviously important.)
So one message to take from this is that if there is evidence of complications, you’re probably outside that 12 hour window, and the balance of decision-making now shifts to ‘how do we take this out in the safest fashion possible?’ rather than ‘how do we take this out in the quickest way possible?’
This makes a heap of sense but initially the safest way possible is also the quickest way possible. (So maybe, the question is always how do we take it out the safest way possible. It’s just about what’s safe at different phases.)
Like every symptom associated with these annoying energy pills, those with complications are not necessarily super specific. All of the following can be part of the picture:
- Blood – haemoptysis, haematemesis, melaena.
- Abdominal pain.
- Weight loss.
- Chest pain.
- Cough/stridor/hoarseness.
Definitely couldn’t be anything else.
Anything that looks like blood needs to be taken particularly seriously. Brumbaugh et al showed that up to 70% of cases of fatal haemorrhage had some form of herald bleed beforehand. When you think through the fact that the presence of bleeding at all has to at least suggest that erosion has happened in the direction of a blood vessel and that the blood vessels in this region are really quite big, it definitely makes sense to be a little worried.
So in that context we turned to the polls again to ask ‘should we get this thing out quickly’ or ‘should we get that kid out (of here) quickly’ because Bara does many things but one thing it doesn’t have is the option for ECMO and that version of cardiac support. And it was a bit more split because this is tricky I guess but on balance 57% of the respondents thought maybe get that kid out.
This kid probably does need cardiac options. It may be that further imaging (say, a CT angiogram) might define what is going on a little better. It might also be that having the option for cardiology intervention with a stent to reinforce at risk areas before retrieval, plus a plan for either pre-emptively initiating cardiopulmonary bypass or peripheral ECMO could be put on the table.
What is guaranteed is a beautiful opportunity to include even more people in the team-based discussion. But to talk to more people you probably need to go somewhere with those more people.
Which is something that can happen just as things are heating up in multiverse 3.

Don’t Miss the Train
In this multiverse, the one created that one time you ran too slowly to get the Gautrain and ended up being serenaded by a banjo player (grim times all around), a grandmother brings her 2 year old in with a history of having a bit of a cough and being off their food.
And possibly due to some weird impulse that seems to have travelled across space and time itself, the patient gets an X-ray which shows a button battery and there is just enough in the story to make people look a little harder with a CT scan.
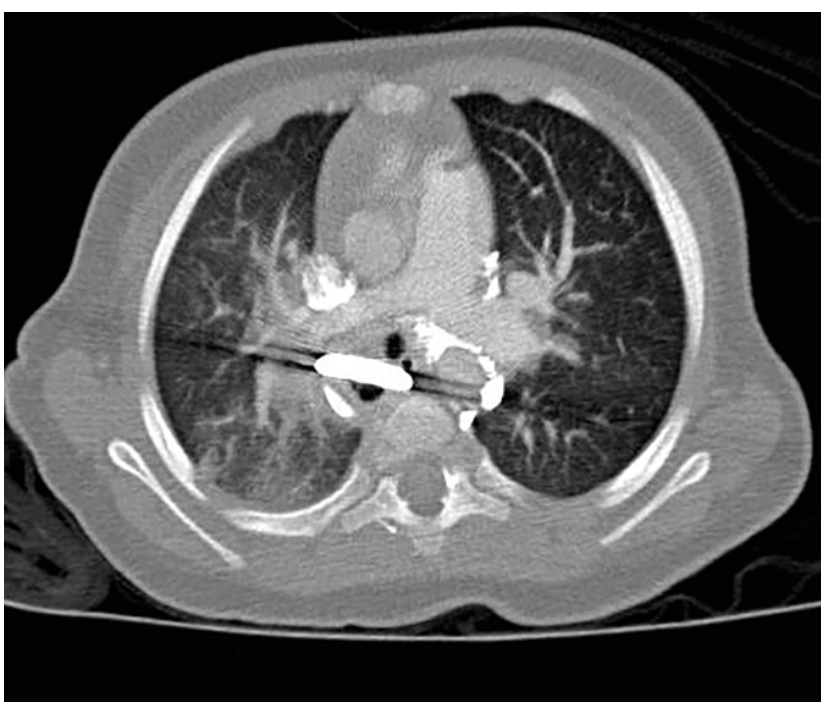
And it’s fair to say that a patient with symptoms of complications possibly weeks down the track a moment for pause is required. Partly because finally we’re back at the part of the talk that is actually about acquired tracheo-oesophageal fistula. Which was supposed to be the point I recall.
Perhaps the thing to do at this point is actually to take a step back from acquired TOF specifically and talk more broadly about anaesthesia for tracheo-oesophageal fistula. It turns out that there isn’t necessarily a lot of agreement on what you should do. A little while back Knottenbelt et al looked retrospectively at TOF anaesthesia across 101 patients in the Oz/NZ context. In their series, 32% had an IV induction, 68% had an inhalational anaesthetic and 64% of the patients were maintained with spontaneous ventilation until control of the fistula.
In a paper put out by Van Hoorn et al, which bizarrely also had 101 patients (but only 86 were induced in theatres), 52 had an IV induction, 30 had sevoflurane and 78 had muscle relaxation (thought it’s a little hard to pick the timing and use of it and 4 of those had suxamethonium. Of interest in this second paper, 75 of the 101 had a desaturation, 28 had a severe desaturation under 80% and 2 had a desaturation under 50. It’s a little hard to be certain given some of the absences in the description, but one of the traditional justifications behind maintaining spontaneous ventilation is that you retain some reserve of oxygenation in a context of knowing that there is always a risk of ventilating the fistula when in a controlled ventilation setting.
In my personal practice this also has always had me wanting a flexible bronchoscope available wherever that’s an option. This is independent of whether the patient has rigid airway endoscopy at the start. That’s because telling you the depth of the fistula with the patient in a supine, neck extended position for rigid airway endoscopy doesn’t necessarily give you up to date information once the patient is on their side for the operative procedure, probably with less neck extension.
And the rigid airway endoscopy at the start probably won’t help if the surgeons are moving the tissues around as part of their operation. So my philosophy tends to be ‘having more information available at times that matter is probably good’. It also makes it easier to try and buy a little extra margin of safety by placing the tip of the ETT in a position not ventilating the fistula, wherever possible. And that confirming it is still there if things change.
So perhaps the overarching philosophy for tracheo-esophageal fistula anaesthesia is really:
“Make a plan with a …”

So in practice there are a couple of key questions:
- How will you maintain oxygenation?
- What happens if it all falls apart?
For the first one we’ve kind of covered that off. At least the folks on the poll did because 86% wanted to keep them breathing. This made life easier for me, because that kind of equates with what I tend to do in practice when I actually get to anaesthetise for these cases. And I think it is actually pretty sensible to do what you do well in your hands when doing things are tricky.
So I would tend to undertake inhalational induction. If the crew are keen on rigid airway endoscopy, I’d still plan to place the ETT with a flexible bronchoscope and by preference place it past the fistula. I’d then re-check position when positioned for the surgery. I’d be thinking of utilising a combination of blocks (the ESP block looks like it may have a role here), ketamine, dexmedetomidine and carefully titrated opioids for analgesia. And I’d deploy muscle relaxation once the join is sorted.
That’s the standard plan anyway. Question 2 is maybe less relevant in congenital TOF but really important in acquired ones because the tissues are probably going to be pretty awful for the surgeons to deal with and the risk of things falling apart. At least in a congenital case there is likely to be some options for oxygenating/ventilating useful bits of lung. If it falls apart here, that may not be so easy to produce restoration of oxygenation/ventiation.
And this may well be why a discussion about doing the whole procedure with cardiopulmonary bypass comes into the mix for these patients. It is described in this Hofmeyr paper, and it is likewise described in a paper covering multidisciplinary care in both the congenital and acquired scenario. In that series 100% of the acquired cases (5/7 being button batteries) were done with cardiopulmonary bypass.
Which brings us back to a core answer useful for many exam scenarios: “Initiate a multidisciplinary team-based discussion to ensure a plan which allows preparation for the rare but serious complication”.
It may be that it is thought that the risk of things going pear-shaped is actually pretty low in which case just having secured wire access to initiate peripheral ECMO before getting on with it might be perceived as reasonable. It seems though, that plenty in this situation would prefer the super controlled version with bypass from the get go.
Which finally brings us back to the super simple summary version:
- If you think it was now get it out.
- If you see blood, assume mayhem.
- If there is a TOF, plan a way out.
And that should help in whichever part of the multiverse you’re in. But maybe try and steer clear of the one where the donuts taste like cat liver.
The Bibliography:
Some of those initial stats come from the National Capital Poison Center in the US. Their section on batteries is here.
These ones describe various elements of presentation/diagnosis/epidemiology:
Now along the ways I mentioned guidelines:
The NCPC one is here.
Here’s an ESPGHAN position paper that is not quite out yet:
A North American variant is this one:
And how about an Italian one here:
Would you like some reading on how the damage occurs and how to mitigate that?
The Soto paper covering perforations is this one:
Another outcomes one?
What about the TOF ones?
And a little on specific acquired TOF/button battery scenarios:
Finally, how about a couple of anaesthetic review type ones:
And if you got this far, maybe you need to be absolutely haunted by these ancient instruments.

Pingback: 3 Batteries in the Multiverse — Songs or Stories – Prehospital and Retrieval Medicine – THE PHARM dedicated to the memory of Dr John Hinds·